



Childhood abuse and neglect have far-reaching consequences, as evidenced by recent studies and outbreaks. A study conducted by the University of Pittsburgh has revealed a concerning link between childhood abuse or neglect and adverse COVID-19 outcomes in adulthood. The study analyzed data from the UK Biobank and found that individuals who reported childhood adversity had a higher risk of being hospitalized for COVID-19 or dying from the virus. The authors of the study propose that the long-lasting effects of early-life trauma, such as inflammation and alterations in the hypothalamic pituitary adrenal axis, may contribute to the increased mortality and hospitalization rates. This research emphasizes the need for further investigation into the relationship between childhood abuse and COVID-19 outcomes [56a012ae].
In China, hospitals are currently grappling with an outbreak of pneumonia among children. This outbreak, which has spread to cities across the country, including Beijing, could be linked to Mycoplasma pneumoniae, also known as 'walking pneumonia'. The surge in cases comes as China enters its first winter without strict COVID-19 lockdown measures. Symptoms of walking pneumonia include a sore throat, fatigue, and a lingering cough. The recent surge in Mycoplasma pneumoniae has raised concerns about growing antibiotic resistance. While there have been no related deaths so far, the situation highlights the importance of monitoring and addressing child pneumonia outbreaks [b143a81b].
The common theme in these two incidents is the lasting impact of childhood trauma on health outcomes. Both the study on childhood abuse and COVID-19 outcomes and the child pneumonia outbreak in China underscore the long-term consequences of early-life adversity. Whether it is the increased risk of severe COVID-19 outcomes or the vulnerability to pneumonia outbreaks, childhood trauma can have a profound effect on health. These incidents call for further research, awareness, and support systems to address the lingering impact of childhood trauma on individuals' well-being and public health as a whole.
Long COVID, the persistence of symptoms after the acute infection has passed, is still a concern. A study on health records from the UK and Spain found that a first infection can cause persistent symptoms, such as altered sense of smell or taste, fatigue, and breathing problems. However, the risk of persistent symptoms is much higher in a second infection. Viruses that leave long-lasting problems are not new, and research shows that while some people recover from long COVID, others experience severe and debilitating symptoms. In the US, there is a rise in the number of people reporting disabilities, which could be related to long COVID. The Australian data also suggests a rise in the rate of people who can't work, potentially indicating the impact of long COVID. It is important not to dismiss the concerns about long COVID and to gather more data before disregarding precautions like wearing masks and avoiding crowds. [5a27c489].
Covid is causing severe infections and prolonged illness in some individuals. Antibody levels against Covid are low, allowing for a higher dose of the virus to cause more severe disease. Waning immunity and the evolution of the virus are contributing to the increased severity. The wide and fast rollout of vaccines last year made a significant difference in reducing illness, but this year fewer people are being offered the vaccine. The Omicron variant and its variants have evolved to be distant immunologically from the original virus, resulting in little immunity. T-cells play a role in preventing severe illness and hospitalization, but their activity can cause muscle pain, fever, and chills. Covid is not yet on a trajectory to become a mild infection, but repeated infections may lead to natural immunity. Overall, Covid is still causing significant illness and may result in a grotty winter for many people.
Sarah Taylor, a lecturer at Keele University, has shared her experience of living with long Covid. She discovered she had the condition in 2022 when she woke up on New Year's Day with symptoms of brain fog and exhaustion. Her symptoms, which included muscle rigidity and difficulty swallowing, prevented her from returning to work. After waiting three months, she was referred to a long Covid clinic where her swallowing ability was assessed. She found that she was unable to swallow foods with different textures, such as cornflakes, due to the difference in crunchiness and liquidity. Another symptom she experienced was difficulty recalling names. Long Covid is a condition where symptoms persist for an extended period of time after the initial infection. The NHS states that most people recover within 12 weeks, but some experience symptoms such as extreme tiredness, shortness of breath, muscle aches, loss of smell, memory problems, chest pains, and difficulty sleeping. [d3c65756].
Exercise therapy as a treatment for long Covid patients has been a topic of discussion. There are potential risks associated with exercise therapy, as highlighted in an article by Bloomberg. The article mentions the case of a woman who experienced a worsening of symptoms after participating in an exercise program. It emphasizes the need for caution and individualized approaches when prescribing exercise therapy for long Covid patients. Further research is needed to better understand the effects of exercise on this patient population [8dda4048].
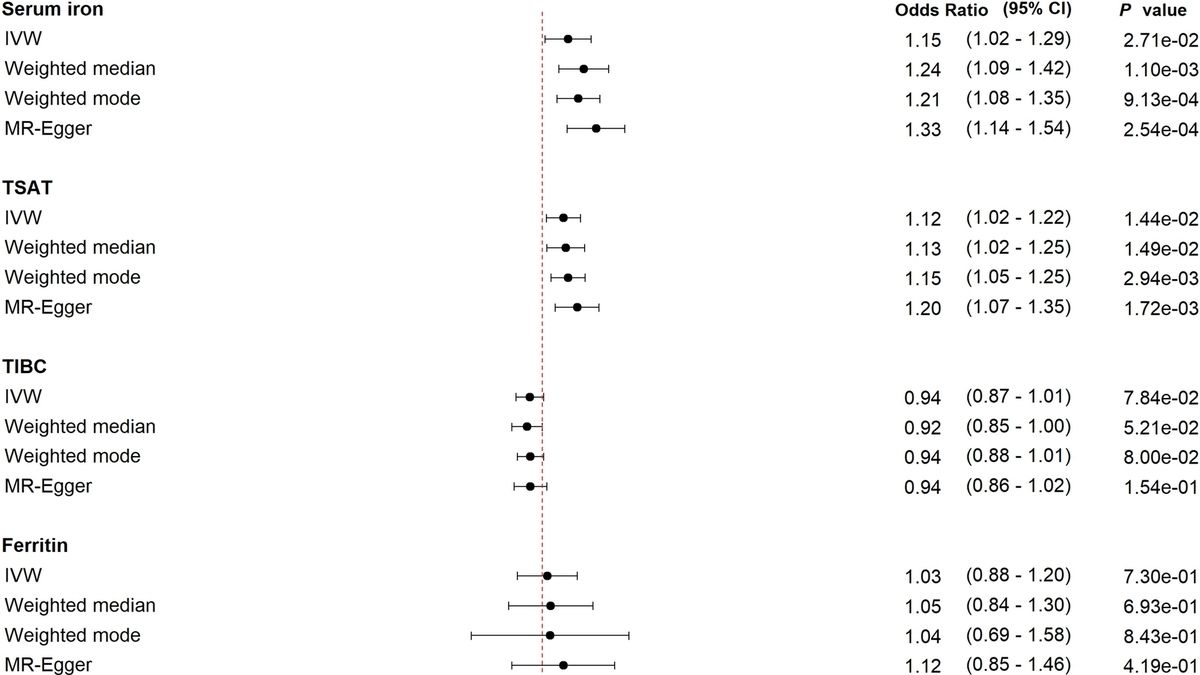
Recent research reveals that low iron levels following a COVID-19 infection are a significant trigger for long COVID. A study by the University of Cambridge found early iron dysregulation in 45% of patients with long COVID symptoms. Iron dysregulation can lead to ongoing inflammation and low iron levels, which may cause the prolonged symptoms experienced by long COVID patients. Scientists face challenges in mobilizing iron back into the bloodstream to alleviate symptoms. Monitoring iron levels and meeting daily iron requirements through diet or supplementation could be vital in managing long COVID. The study opens up potential pathways for prevention and treatment by addressing iron dysregulation early in the infection. Further research is needed to develop effective strategies for managing iron levels in COVID-19 patients. The breakthrough study offers hope for those affected by long COVID and contributes to a better understanding of the condition [b4f9c349].
Some people are more prone to severe COVID-19 due to genetic factors. A study published in the journal Nature found that a gene called TYK2 plays a role in the body's immune response to the virus. People with certain variations of the TYK2 gene are more likely to develop severe symptoms. Another study published in the journal Science Translational Medicine found that a gene called OAS1 also affects the body's immune response to the virus. People with certain variations of the OAS1 gene have a higher risk of severe COVID-19. Understanding these genetic factors can help identify individuals who are at higher risk and develop targeted treatments [657fccd8].